FYIs about HIE
If you already know what Hypoxic-Ischemic Encephalopathy (HIE) is, it was probably a terrifying experience that brought you to this information. For this, I see you and I feel for you. For those who don’t know what HIE is, I hope to educate you and make you more aware of this condition, as April is HIE awareness month. HIE is estimated to occur somewhere between 2-9 in every 1,000 births, and this diagnosis accounts for approximately 8% of all admissions at the hospital I work at. This means that babies with HIE make up a large part of my caseload in the NICU. It also means that the babies/families it affects, as well as effective treatments for HIE, are near and dear to my heart.
FYI: This post is full of lots of dense information, so take your time reading through it and use it a resource to reference—there is lots of good information linked throughout as well!
What is HIE?
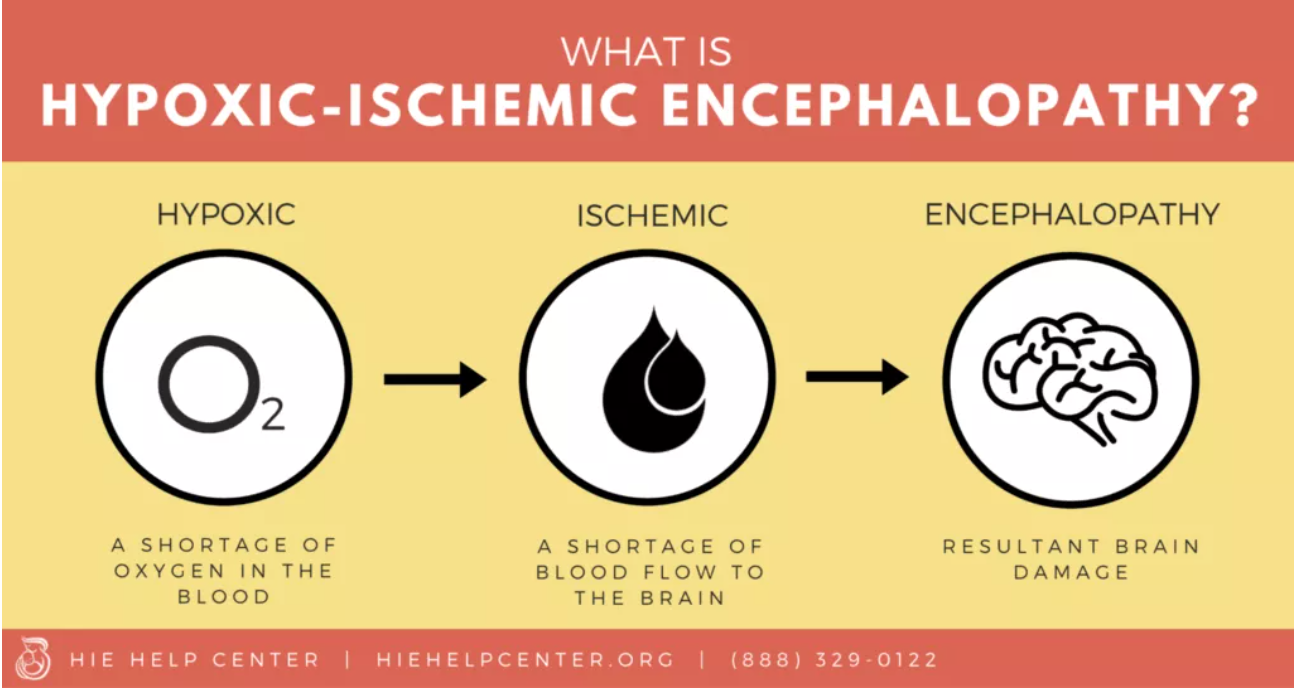
Hypoxic Ischemic Encephalopathy (HIE) happens when there is a lack of blood flow and oxygen to the brain during birth. The short of it is that HIE results in injury or damage to the baby’s brain. The long of it is why I am writing this post. Each baby’s journey with HIE is different, and depends on a multitude of factors. There is a lot about HIE that is unknown, unpredictable, and uncertain, as the brain is a complex and ever-evolving system, especially in little ones.
HIE can happen for a variety of reasons, including umbilical cord issues (also sometimes called neonatal asphyxia), poorly managed pregnancy complications (including gestational diabetes and preeclampsia), failure to monitor fetal vital signs during the birth process, and infection, among other things. It commonly results in respiratory distress or breathing issues at birth. In the delivery room, babies are given an Apgar score at 1, 5, and sometimes 10 minutes of life. This score indicates the baby’s overall stability by looking at heart rate, breathing, muscle tone, color, and reflex responsiveness. A low Apgar score is cause for concern, and often the first indicator that a baby might have HIE.
While no parent ever hopes to find themselves in the NICU, in the case of birth injury or trauma, it is the best place for your baby to be. A neurologist will invariably join your baby’s team and will be a key player throughout the admission to closely monitor baby’s brain and neurologic function. If HIE is suspected, an EEG will likely be started to watch closely for seizure activity. We are learning so much about it and how to best support babies with HIE all the time, but one thing we do know for sure is that intervening EARLY is key for optimizing outcomes.
Therapeutic hypothermia
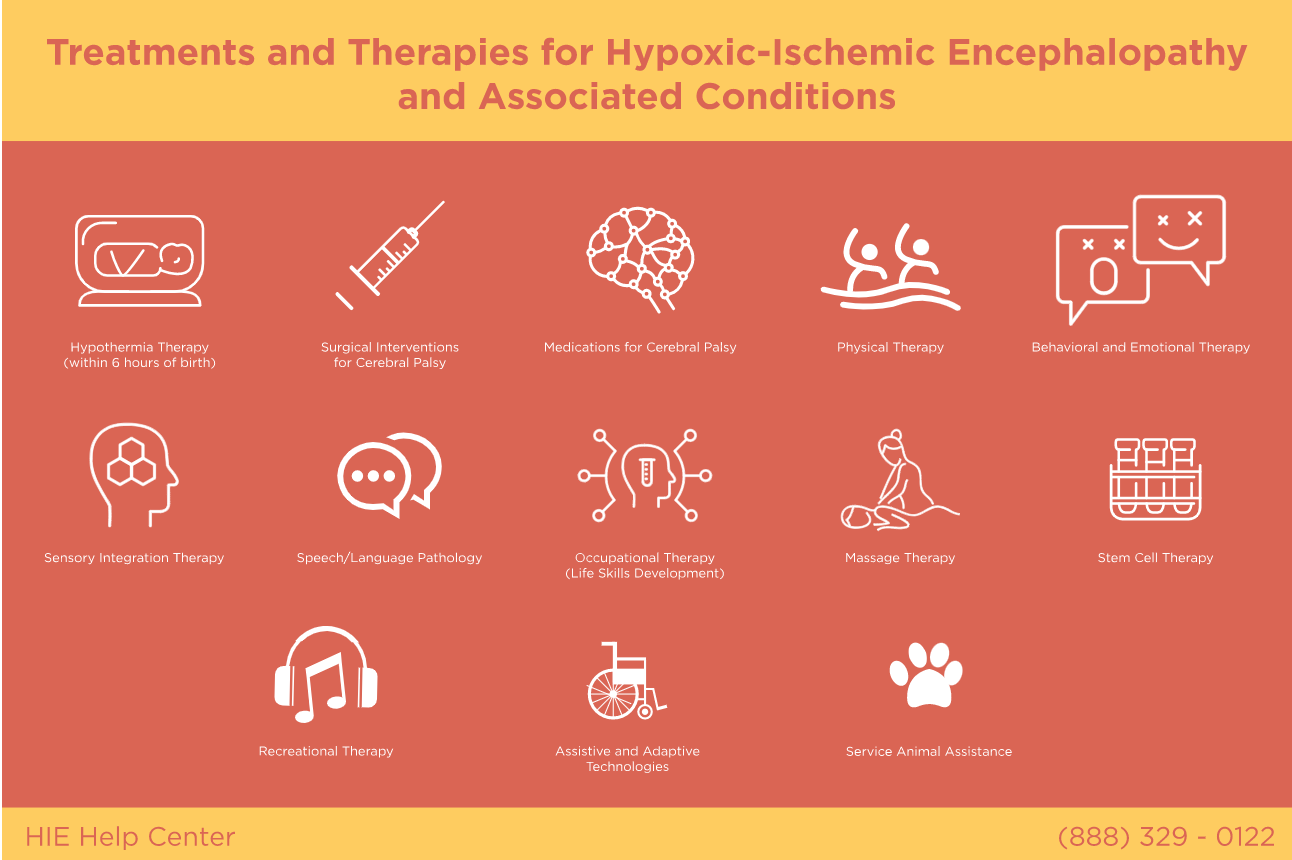
Medical advancements have come a long way in regards to the treatment of HIE. Therapeutic hypothermia, or cooling therapy, has been shown to reduce the impact of brain injury if initiated early (ideally within 6 hours of life). It consists of actually cooling the baby’s temperature (either just the head or the whole body) to 33.5 degrees C (about 92 degrees F) for 72 hours. This allows the brain to heal, pauses metabolic processes, and reduces the sequelae of injury to the damaged brain. After the 72 hours, baby will slowly be re-warmed to baseline body temperature. Your neurologist will be a key player here to monitor for and treat seizures as baby is re-warmed.
Baby is re-warmed…now what?
Your medical team is about to grow! Now that baby is re-warmed, a series of specialists will be popping by to examine and support your baby depending on their needs. They usually will have a feeding assessment to look at suck and swallow efficiency and safety, will have brain imaging via a CT and/or MRI to further examine the extent of damage to the brain, and physical therapy (heyyyy, it’s me!) will come onboard to evaluate and support motor development.
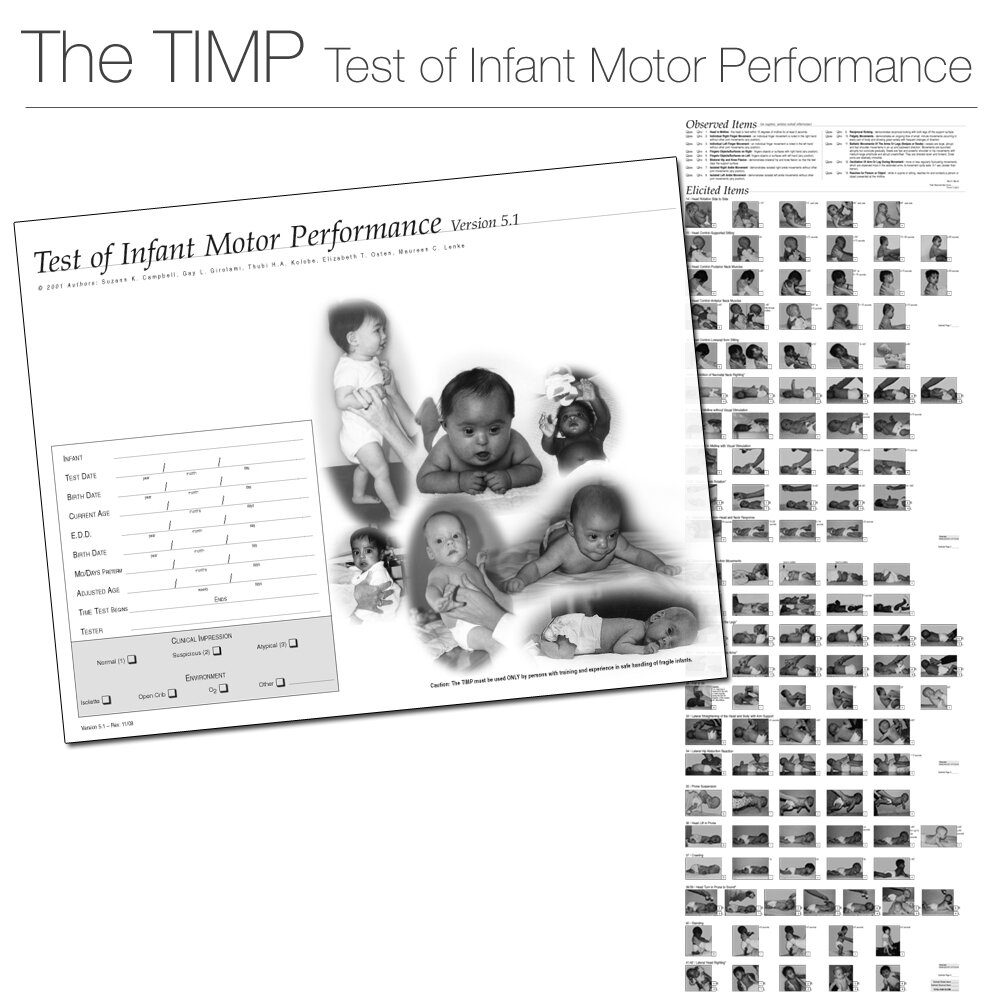
We know that babies with a history of HIE are at higher risk for neuromotor impairments (specifically cerebral palsy) and developmental delay. In our NICU, these babies are placed in a high-risk category and are given a series of assessments during their hospital admission and after discharge to keep a close eye on their development. I perform standardized assessments that look at muscle tone, reflexes, postures, and responses and give us an idea of their developmental baseline. Often, the effects of HIE don’t show up until later when babies demonstrate delayed motor milestone development (more on that here), so it is important to have ongoing check-ins to track and support growth. In our area, babies are seen at 3, 6, 9, and 12 months for developmental assessments and check-ups with neurology and a developmental pediatrician. This allows us to track baby’s progress over time and identify areas of support that are needed. A PT will perform a series of tests (such as the TIMP listed below) to formally document a baby’s developmental trajectory.
Early intervention is key
I mentioned the need to intervene early via cooling therapy, but the importance of early action to support babies with HIE extends beyond just the physiologic brain healing process. Starting therapies in the NICU (OT/PT/SLP, etc.) helps get development off to a strong start and lays the groundwork for monitoring growth. After discharge, early intervention programs across the nation are available to babies at risk for or with identified developmental delays. OT, PT, speech therapists, teachers, and other specialists will team together to best support your baby’s individual needs and goals during those first critical years of development.
I loved working in early intervention and helping babies and toddlers during their critical first years of development!
Hope for HIE
A birth story that includes HIE is often scary, unpredictable, and traumatic. Reach out to your loved ones for support, seek help from social work or a therapist, and make sure to take time for yourself in order to process this journey. Remember that you are not alone, and with advancements in medical treatment and care, we are better prepared than ever to help your baby heal and instill hope for HIE.
TL;DR
Hypoxic Ischemic Encephalopathy (HIE) is a diagnosis commonly seen in the NICU setting. It describes injury or damage to the brain that occurs as a result of lack of oxygen and blood flow to the brain. It can happen for a variety of reasons, including birth trauma, poor management of pregnancy complications, infection, or inability to properly monitor fetal vital signs during labor and delivery.
If HIE is suspected, therapeutic hypothermia, or cooling therapy, will take place for 72 hours to help the brain heal and recover.
The NICU team will likely include a neurologist and other specialists to monitor and treat your baby. Therapies will start in the NICU as well to establish baselines and lay the groundwork for development.
HIE places babies at risk for neuromotor impairments (such as cerebral palsy) and developmental delay, so ongoing monitoring of development and early intervention therapy is key!
A birth history that includes HIE can be traumatic and challenging. Seek support, and remember you are not alone—there is hope for HIE!